Abstract
Introduction: Fall prevention measures are a hallmark of high-quality hospital care worldwide. Many of the same risk factors for falls in an acute hospital setting contribute to falls in a behavioral health unit. However, some risk factors are unique to the inpatient psychiatric setting. Factors include the expectation for increased mobilization on an inpatient psychiatric unit, extrapyramidal side effects of medications, orthostatic hypotension as a side effect of medication, inability to use devices such as walkers and canes on psychiatric units because of safety concerns. The current quality improvement study (QI) was designed to investigate the effectiveness of the DMAIC (Define, Measure, Analyze, Improve, Control) approach to reduce falls in the inpatient psychiatric setting.
Method: A prospective study was designed to eliminate the risk of falls by using the Six Sigma DMAIC approaches during January-December 2018. The frequency of falls in every quarter was an index used to determine the efficacy of implementing DMAIC to prevent falls. The study was defined in three phases: a Measurement and determination of baseline data and identification of the potential causes of falls, b) Collection of all fall data during 2018 and analysis of the data, c) Development of strategies and offering recommendations to decrease future falls.
Results: There were a total of 82 falls in 2018. Frequency of falls reduced from 27 in the first quarter of 2018 to 12 (decrease 44 %) in the fourth quarter. Most of the falls happened in the first three days of admission. The most common time for a fall was between 9 am and 10 am and, 86% of falls did not result in injury.
Keywords
DMAIC, Fall, In patient psychiatry
Introduction
Fall prevention measures are a hallmark of high-quality hospital care throughout the world. Patients at high risk for falling are often designated with unique wrist bands, signs over their bed and outside their hospital room, and even assigned to hospital staff who sit at the bedside and provide constant observation [1]. The underlying etiology of falls is often apparent: altered sensorium attributable to unfamiliarity with the environment, illness, injury, and the effects of medications/treatments [1]. A single fall might cause a patient to become fearful of falling and reduce their mobility, precipitating the loss of function and putting them at higher risk for more falls. Injurious falls lengthen hospital stays, increase the cost of hospitalization, and result in poorer patient outcomes. The risk factors for falls in an acute hospital setting also apply to patients hospitalized for psychiatric reasons. However, there are additional risk factors for patients on a psychiatric unit. While patients on a medical unit are confined mainly to their bed or a nearby chair, patients on psychiatric units are usually more active. Instead of food and medication brought to them, they typically get medication from a nursing station and eat cafeteria-style meals in a dining room. They also watch television in a common area, attend group activities, exercise, and interact with peers. All of this amounts to an increased level of ambulation. Additionally, the average length of stay on a behavioral health unit is longer than a medical admission [2]. Add to the myriad of potential side effects and adverse reactions to psychotropic medication (antidepressants, antipsychotics, sedative/hypnotics, etc.), which may potentiate confusion or agitation and impaired gait or balance, extrapyramidal side effects, and orthostatic hypotension, among other adverse reactions [2]. The combination of psychiatric de-compensation, increased ambulation relative to other parts of the hospital, and treatment effects induce an increase in falls in the inpatient psychiatric unit.
Several causative factors were identified to reduce the occurrence of these falls in hospitals. These include inadequate staff communication, incomplete orientation, and training; incomplete patient assessments and reassessments; environmental issues; incomplete care planning and unavailable or delayed care provision; and inadequate organizational culture of safety [3]. These factors need to be explored by conducting a root cause analysis to implement an appropriate falls prevention program to prevent and reduce the fall rate in hospital settings [4].
Utmost care needs to be taken while formulating a customized falls prevention program specific to a particular setting that focuses on a standard assessment of risk factors, universal fall precautions including scheduled rounding protocols, post-fall procedures such as clinical review, and its root cause analysis.
While implementing these fall prevention programs, hospital administrators utilize several approaches to reduce falls and enhance patient safety [5]. One such approach is Six Sigma. Six Sigma is a robust and validated methodology for quality improvement, cost reduction, and enhancing efficiency by using quantitative analysis and taking customer experience into account [6].
Define, Measure, Analyze, Improve, and Control (DMAIC) is part of the Six Sigma techniques, a data-driven improvement process used to optimize standard operating procedures in a given operational system [7]. It was initially developed for the engineering and production industry and is becoming an increasingly popular tool in many other industries, including healthcare.
This approach is executed in five phases: defining opportunities (D); measuring performance (M); analyzing opportunities (A); improving existing performance (I); and control of the improved performance (C). Previous studies demonstrated the effectiveness of the DMAIC approach to reduce patient falls in various clinical settings [5,6,8]. The current quality improvement (QI) study was designed to investigate the effectiveness of the DMAIC approach in an inpatient psychiatric unit.
Methods
This study was conducted at a large metropolitan hospital with 78 adult inpatient beds, divided into three identical psychiatric inpatient units, all of which run autonomously, with their own dedicated nursing staff and specifically assigned physicians. Each unit has 26 beds in either single or double occupancy rooms. The rooms have their own bathroom (sink, toilet, and shower). The unit also has an activity room, where group activities are run throughout the day, led by various therapists, and a dining room where patients assemble for three meals per day. There is also a nursing station on each floor, staffed 24 hours per day, where patients receive their medication.
A prospective study was designed to eliminate the risk of falls and create a safe environment for both patients and healthcare professionals by using the Six Sigma DMAIC approach between January and December 2018. The frequency of falls in every quarter is an index used to determine the efficacy of implementing DMAIC to prevent falls in the present study. Data was collected throughout the year but reviewed retrospectively at the end of the year.
The study was defined in three phases: ?) Measure and determine baseline data regarding falls in inpatient psychiatry and identify the potential causes of the fall. ??) Collect all fall data during 2018 and analyze the data ???) Develop strategies and make recommendations to decrease future falls.
To execute the study, a multidisciplinary team with all the relevant stakeholders was formed. The team consisted of representatives from the risk management, nursing, and resident and attending physicians.
All falls, either reported by the patients or observed by the staff, occurring in these inpatient units from January 1 to December 31, 2018, were reviewed as part of this study. Data sources include incident reports, fall response team reports, nursing performance improvement forms, and Fall Analysis/Debrief forms, along with a review of the patient’s chart. IRB approval was obtained for this project. All possible causes and risks were identified through various meetings held with the team. Based on the cause and effect diagram findings, the team categorized potential reasons for the occurrence of falls into five categories (Figure 1).
Figure 1: Cause and effect diagram showing possible causes for patient falls.
In the analysis phase, the causes that were identified for all falls during a year were taken into consideration, and appropriate strategies were developed through several sessions with stakeholders. The preventive strategies were implemented in order when they developed.
Data include age, sex, time of fall, day of admission, injury, location of the fall, patient-level of fall risk, alcohol withdrawal symptom, narcotic withdrawal symptom, psychiatric diagnosis and medical comorbidity. Each fall was categorized as having either no associated injury or minor, moderate, or major injury. Death was also a category of injury. The minor injury required minimal treatment, including applying ice or cleaning a minor wound or laceration. Moderate injuries were ones requiring sutures or steri-strip/glue. Major injuries included falls with any fracture or those requiring surgery or casting. According to Morse fall scale, the level of risk is defined as high risk and standard of risk.
Results
82 falls registered in 2018 in the three inpatient psychiatric units.
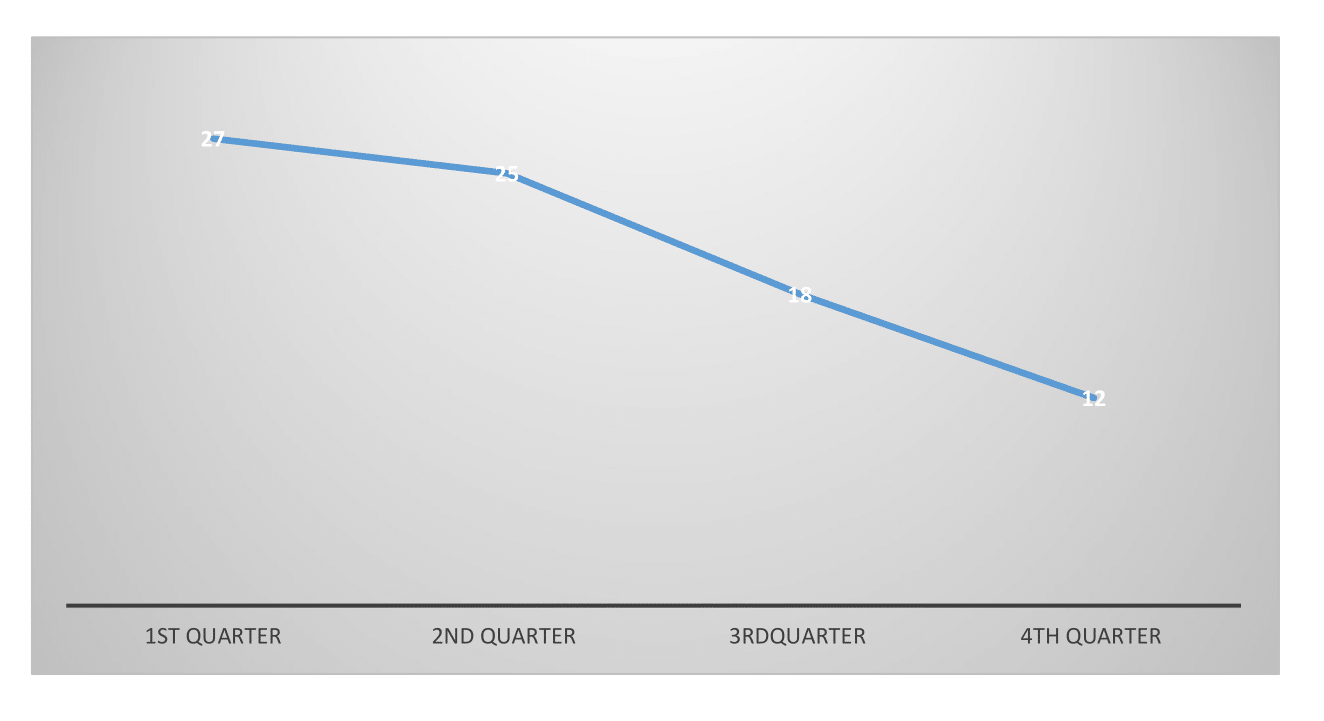
Implementing DMAIC reduced the frequency of falls from 27 to 12 (44%) from the first quarter of 2018 to the fourth quarter (Figure 2).
Figure 2: Frequency of fall in every quarter in 2018.
Characteristics of patients with falls are shown in Table 1.
20 % of the patients were on sedative/narcotics before fall, and 5% were in alcohol withdrawal. 5% of the cases were on Suboxone and 10% on Methadone.
|
Characteristics of Patients with Fall |
|
|
Total Number of Falls |
82 (59.3% female, age 44 ± 19 years) |
|
Most common day that a fall occurs |
Day 1-3 of admission |
|
Most common time of day that a fall occurs |
9-10am (19%), 3 pm, (6%) and 8 pm (6%) |
|
Injury due to fall |
85% No injury noted 5% Head and Face 2 % Lower Extremity,7 %Upper Extremity 1% Lower back |
|
Observation level at time of fall |
33% Every 15-minute checks, 2.5 % 1;1 observation |
|
The average length of stay
|
11 ± 20 days |
|
A most common location for fall |
32% in the hallway, 20% in the bathroom, 16% in their own room, 13% proximity to their bed, 19% in another place on the unit |
|
Continuous status |
24 % alert, 4% confused and 72% alert and oriented. |
|
Medical history |
63% has no history of falls or medical issues, 13% have unsteady gait, 4% previous history of falling, 11% history of hypertension, and 17% dizziness before falling. |
|
Environmental risk factor |
93% no risk factor, 7 % wet floor
|
|
The location that falls accrued from |
10% bed, 1% commode, 54% while ambulating in the unit, 5% from the chair, 4 % in the shower, and 27 % from other places |
|
Psychiatry Diagnosis |
24 % substance use disorder, 11% major depressive disorder, 11%scizoaffective disorder, 5% bipolar disorder 12% schizophrenia, 37% no diagnosis registered
|
|
Treatment after fall |
87% no need for treatment, 4 % needed X-ray, 1% Suture, strip, glue, splinting, and 8% needed dressing, cleaning the wound, ice, limb elevation, and topical. |
Discussion
In the current study by using DMAIC, we identified all possible risks and causes falls on an inpatient psychiatric setting. Strategies listed in table 2 developed which were implemented and monitored at every quarter. The study demonstrated that using DMAIC can reduced and prevent fall significantly on in patient psychiatry setting.
Among the most heartening pieces of data extrapolated from this study was that 98% of falls experienced in the inpatient psychiatric unit resulted in either no injury or minor injury. This would imply the modern-day inpatient psychiatric unit is largely well-planned to avoid serious repercussions from falls. Among the most significant findings in this study is that 19% of falls occurred between 9:00 AM and 10:00 AM. This is most likely attributable to a phenomenon known as sleep inertia, a period of transitory hypervigilance, confusion, disorientation of behavior, and impaired cognitive and sensory-motor performance that immediately follows awakening [9]. In an average person, this period might last between 15 to 30 minutes [10]. However, in a hospitalized patient, sleep inertia may persist for hours. It is reasonable to believe this condition may potentially become exacerbated in the context of medical issues like aberrant glycemic levels, fluctuations in blood pressure, and other medical comorbidities typical of hospitalized patients.
All of this, in addition to the psychiatric exacerbation that necessitated hospitalization in the first place. The most effective method of counteracting the influence of sleep inertia on fall risk is for treatment team members and hospital staff to be vigilant during early morning hours when patients are most vulnerable to falls. In addition to obtaining vital signs and blood sugar levels, it’s essential to assess a patient’s mental status soon after they wake. If required, patients should be assisted with using the restroom, personal hygiene, taking medication, and eating breakfast.
Our data showed that fall incidence increases in the first three days of admission. One of the most frequently occurring risk factors of falls is confusion, disorientation, and unfamiliarity with the unit [11,12], which are more common in the earlier part of an admission. Fall risk must be assessed not only at the time of admission to the inpatient but also every day throughout the length of stay. It should be a routine component of the discussion during the morning report and all nursing handoffs and shift changes. Several instruments are used clinically to estimate a patient's risk of falling. The STRATIFY (Oliver, Britton, Seed, Martin, & Hopper, 1997), the Morse Fall Scale (Morse, Black, Oberle, & Donahue, 1989), and the Hendrich II Fall Risk Model (HIIFRM) (Hendrich, Bender, & Nyhuis, 2003) are three instruments widely used in clinical practice by nurses. The Morse Fall Scale was used in the current study, but 73% of patients were identified as low risk.
The differences between patient groups based on medical diagnoses suggest the instrument does not perform equally across patient groups, nursing skill levels, or clinical units. The study showed the clinical concern remains that many patients who fell were scored as low risk using the HIIFRM instrument [13]. The Heindrich II Fall Risk Model is potentially helpful in identifying patients at high risk for falls in acute care facilities [14]. The STRATIFY scale was found to be the best tool for assessing the risk of falls by hospitalized acutely-ill adults. However, using these instruments varies considerably depending on the population and the environment, so their operation should be tested before implementation [15]. More studies need to be done to determine which screening tool has more accuracy in inpatient psychiatric units.
The key to preventing falls among hospitalized patients may lie in addressing how the hospital environment creates risk. Nurses should continue to improve the ability to assess fall risk and implement interventions that modify or eliminate risk when possible. The patients admitted to an inpatient psychiatric unit are generally younger than patients on a medical unit and are more ambulatory in the unit. However, they may be prescribed psychotropic medications, which have sedative effects, putting them at a higher risk of falls than other patients.
Our study showed that patients fall in the hallway more than in any other area, and this is likely because the hallway is a high-traffic area. Patients often pace the hallways as a means of passing the time or relieving anxiety. The incidence of falls on psychiatric units in the elderly tends to be higher than on medial units, with estimated rates of 13.1 to 25 per 1,000 inpatient days compared to 3 to 5 per 1,000 inpatient days, respectively. Falls in the elderly on inpatient psychiatric units have serious adverse outcomes resulting in injuries such as fractures, head trauma, and death. Even mild fall-related trauma may result in a prolonged hospital stay [6]. There is an increased risk of falls among individuals with cardiovascular disease [16]. Knight et al. [17] found significantly higher heart rates for patients who fell in a psychiatric unit. Increased heart rate may be an indicator of fall risk. So, strategies such as identifying cardiovascular disease and other medical comorbidities, medication review, and assessing gait instability may help prevent falls [18].
Conclusion
Patients on an inpatient psychiatric unit are at increased risk for falls, and this relates to several factors, including (1) the nature of a psychiatric ward, which promotes ambulation, (2) increased risk from psychotropic medications and (3) sleep inertia. The results in the current study give credence to a DMAIC approach to reducing fall risk in inpatient psychiatry, and the broader implementation of this method would likely yield similar results in other settings. Table 2 shows some strategies to prevent falls in inpatient psychiatry.
|
|
|
|
|
|
|
|
|
|
|
|
References
2. Zhang J, Harvey C, Andrew C. Factors associated with length of stay and the risk of readmission in an acute psychiatric inpatient facility: a retrospective study. Australian & New Zealand Journal of Psychiatry. 2011 Jul;45(7):578-85.
3. The Joint Commission, Strategies for addressing the root causes of falls. In Smith, I.J. (Ed.), Reducing the Risk of Falls in Your Health Care Organization, Joint Commission Resources, Oakbrook Terrace. 2005;29-50.
4. National Quality Forum, National voluntary consensus standards for nursing-sensitive care: an initial performance measure set, National Quality Forum, Washington, DC, (2004), available at: www. qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier (accessed February 18, 2016)
5. Al Kuwaiti A, Subbarayalu AV. Reducing patients’ falls rate in an Academic Medical Center (AMC) using Six Sigma “DMAIC” approach. International journal of health care quality assurance. Int J Health Care Qual Assur. 2017 May 8;30(4):373-384.
6. Goldsack J, Bergey M, Mascioli S, Cunningham J. Hourly rounding and patient falls: what factors boost success?. Nursing 2022. 2015 Feb 1;45(2):25-30.
7. Ahmed S. Integrating DMAIC approach of Lean Six Sigma and theory of constraints toward quality improvement in healthcare. Reviews on Environmental Health. 2019 Dec 1;34(4):427-434.
8. Christopher DA, Trotta RL, Yoho MA, Strong J, Dubendorf P. Using process improvement methodology to address the complex issue of falls in the inpatient setting. Journal of Nursing Care Quality. 2014 Jul 1;29(3):204-214.
9. Ferrara M, De Gennaro L. The sleep inertia phenomenon during the sleep-wake transition: theoretical and operational issues. Aviation, Space, and Environmental Medicine. 2000 Aug 1;71(8):843-848.
10. Tassi P, Muzet A. Sleep inertia. Sleep Medicine Reviews. 2000 Aug 1;4(4):341-53.
11. Khurshid T, Lantz MS. Falls and inpatient geriatric psychiatry: a simple solution to a chronic and difficult problem. The American Journal of Geriatric Psychiatry. 2016 Mar 1;24(3):S90-1.
12. Tsai YF, Witte N, Radunzel M, Keller ML. Falls in a psychiatric unit. Applied Nursing Research. 1998 Aug 1;11(3):115-21.
13. Swartzell KL, Fulton JS, Friesth BM. Relationship between occurrence of falls and fall-risk scores in an acute care setting using the Hendrich II fall risk model. Medsurg Nursing. 2013 May 1;22(3):180-187.
14. Kim EA, Mordiffi SZ, Bee WH, Devi K, Evans D. Evaluation of three fall‐risk assessment tools in an acute care setting. Journal of Advanced Nursing. 2007 Nov;60(4):427-35.
15. Aranda-Gallardo M, Morales-Asencio JM, Canca-Sanchez JC, Barrero-Sojo S, Perez-Jimenez C, Morales-Fernandez A, et al. Instruments for assessing the risk of falls in acute hospitalized patients: a systematic review and meta-analysis. BMC Health Serv Res. 2013 Apr 2;13:122.
16. Darowski A, Chambers SA, Chambers DJ. Antidepressants and falls in the elderly. Drugs & Aging. 2009 May;26(5):381-94.
17. Knight M, Coakley C. Fall risk in patients with acute psychosis. Journal of Nursing Care Quality. 2010 Jul 1;25(3):208-15.
18. Healey F. A guide on how to prevent falls and injury in hospitals. Nursing Older People (through 2013). 2010 Nov 1;22(9):16.