Abstract
Purpose: To determine whether the lesioned hemisphere and the frequency of physical and occupational therapy sessions in inpatient rehabilitation have effects on the functional independence of stroke patients.
Methodology: A retrospective chart review of 165 individuals who underwent intensive inpatient rehabilitation following an acute stroke. The patients received skilled occupational and physical therapy 5 days a week or greater at an intensive rehabilitation facility following an acute stroke. Functional independence was measured using the Functional Independence Measure (FIM) motor score upon admission and discharge. Linear regression analyses were used to determine if there is a significant FIM motor score change depending on the side of the lesioned hemisphere and/or the frequency of therapy sessions.
Results: A significant difference in functional independence as measured by FIM motor score was found when comparing the frequency of therapy for left sided strokes (left stroke 7 days a week versus left stroke less than 7 days a week) (p=0.021). There was no significant difference in FIM motor score change during comparison of other groups: lesioned hemispheres (right vs. left) (p=0.706), frequency of therapy for right strokes (right stroke 7 days vs. right stroke less than 7 days) (p=0.765), or frequency of therapy and side of lesion (right stroke 7 days vs. left stroke 7 days and right stroke less than 7 days vs. left stroke less than 7 days) (p=0.138).
Conclusions: The study suggest that acute left stroke survivors may benefit from intensive physical and occupational therapy, 7 days a week in an inpatient rehabilitation facility, to improve functional independence. Further research is needed to determine any confounding variables which may explain why no significant improvement was noted with increased frequency of therapy for right stroke survivors.
Keywords
Stroke, Hemisphere, Rehabilitation, Independence, Outcomes
Introduction
Stroke is the 5th leading cause of death and the leading cause of long-term disability in the United States [1]. Every 40 seconds, someone in the United States sustains a stroke, resulting in approximately 133,000 deaths per year. Stroke related deaths accounted for 11.8% of total deaths in 2015, making stroke the second leading cause of death worldwide, second only to heart disease [1]. Functional limitations after a stroke can be life altering, resulting in impairments in strength, ambulation, cognition, language and overall independence level [2]. Of those who survive a stroke, about one third will be functionally dependent after 1 year. Most survivors will be admitted to inpatient rehabilitation facilities, with 26% ending up institutionalized in a nursing home [2].
It is known that right and left strokes present different clinically based on the affected region of the brain. Those who suffer from a lesion to their dominant hemisphere, often left sided brain lesions, have been found to present with right sided hemiparesis and hemisensory loss, aphasia, difficulty planning and sequencing movements, and trouble processing verbal cues [2,3]. Those with left sided lesions, also tend to be more aware of their deficits and therefore more cautious during mobility [2]. Aside from left sided hemiparesis and hemisensory loss, non-dominant hemisphere lesions, most often right hemisphere strokes, exhibits perceptual and visuospatial deficits [4,5], while 82% present with visual neglect [6]. Those with right sided lesions often experience decreased awareness of their deficits [2,7] and manifest impulsive behavior [2]. There is conflicting research regarding whether the side of the brain which is affected by stroke has an impact on functional independence. Lopes et al. found no significant difference in balance, gait and functional independence when comparing right versus left hemisphere lesions [8]. A separate study by Bindawas et al. indicated that subjects with right brain lesions exhibited significantly higher functional recovery compared to those with left brain lesions [9]. While Denes et al. found that patients with right sided lesions, demonstrated decreased levels of independence and social adjustment than those with left sided lesions [10]. There is conflicting evidence on the risk for falls with clinical finding showings increased risk of falls in both hemispheres [11-13].
There is a conflicting evidence on the influence of frequency and duration of physical and occupational therapy on functional independence following a stroke. A systematic review by Peiris et al. on patients with stroke, cardiac, orthopedic and other neurologic conditions in which the participants received increased number of therapy sessions and duration of physical and occupational therapy, found that those who received increased amount of therapy demonstrated improvement in walking ability, activity and quality of life, without significant change found in the ability to perform self-care [14]. A systematic review by Kwakkel et al. found a small, but statistically significant improvement of impairments and disability for stroke patients who have undergone increase intensity of therapy [15]. However, studies conducted by the Glasgow Augmented Physiotherapy Study (GAPS) Group and by Blennerhassett and Dite reported inconclusive findings regarding whether increased participation in physical therapy improved functional outcomes following a stroke [16,17].
To our knowledge, there is no research that examines whether the affected brain hemisphere and the frequency of therapy play a role in improvement of functional independence in stroke patients. This study may assist in determining whether the location of the lesioned hemisphere or whether the frequency of physical and occupational therapy sessions have effects on the functional independence of stroke patients. The purpose of this study is to determine whether the location of the lesioned brain hemisphere and the frequency of physical and occupational therapy sessions have effects on the mobility and independence of stroke patients undergoing inpatient rehabilitation.
Methods
A retrospective analysis was conducted using patient records from a hospital system in the greater Orlando, Florida area. The study was reviewed and approved by the Orlando Regional Medical Center Institutional Review Board and was reviewed and acknowledged by the University of Central Florida Institutional Review Board to protect the privacy and welfare of human subjects.
A master list of patients diagnosed with stroke and have underwent inpatient rehabilitation was obtained from the hospital system. From the list of 182 patients, charts were elected for inclusion in the study if at the time of referral to inpatient rehabilitation, the person had been at least 60 years old and was admitted or transferred to a primary stroke center between May 2017 and April 2018 with a final diagnosis of stroke recorded upon admission. Charts were excluded if they were coded as a bilateral hemisphere stroke, other, or no paresis, in order to specifically look at the effects of right versus left hemisphere lesions on functional outcomes. Records are identified in this study by the side of their lesioned hemisphere.
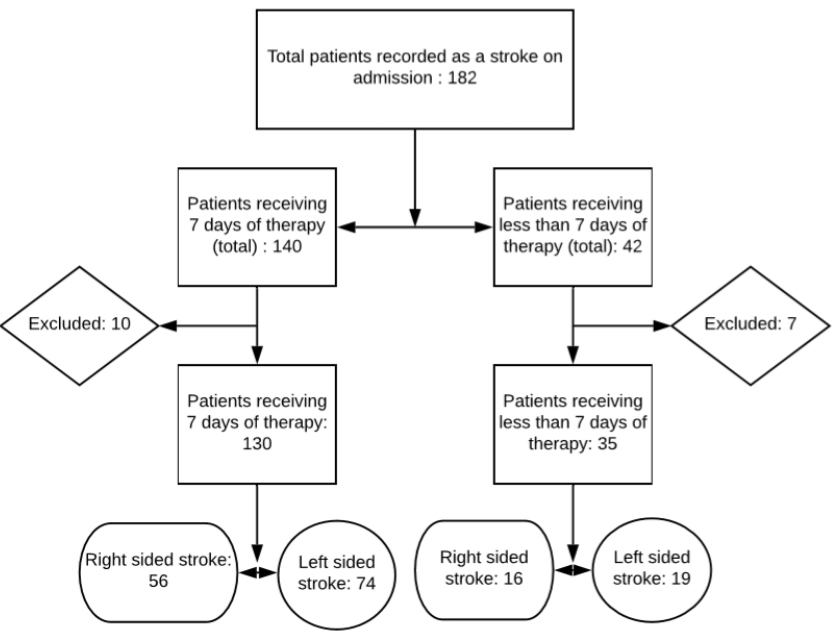
Following inspection of the master list, 165 charts were selected for inclusion in the study. The charts were divided into those who received 7 days of therapy (physical and/or occupational) per week (n=130) and those who received less than 7 days of therapy per week (n=35). The records were further divided into right and left strokes who received therapy 7 days of therapy per week (right n=56, left n=73) and less than 7 days of therapy per week (right n= 16, left n= 19) (Figure 1).
Figure 1: Patient inclusion and exclusion algorithm. Flow chart of the inclusion/exclusion criteria for the study sample.
Data Collection Tool and Outcome Measure
A computer-based data extraction sheet was developed by investigators for use with the patients’ medical records. The data collection form was designed to collect information including age, diagnosis, side of the lesioned hemisphere, frequency of physical and/or occupational therapy session and Functional Independence Measurement (FIM) as the outcome measure for independence. The FIM is an outcome measure consisting of 13 motor and 5 cognitive tasks (18 total task). The motor component consists mainly of activities of daily living (ADLs), transfers and locomotion. For each task, the test is scored on a seven-point scale ranging from total dependence to total independence. The lowest possible total score is 18 and the highest total score is 126 (lowest motor score being 13 and highest being 91), indicating the individual’s current level of independence and burden of care. The FIM has been validated in the stroke population [18] and has been found to have a minimally clinical important difference (MCID) total score change of 22 points, motor score changes of 17 points and cognitive score change of 3 points [19]. The MCID represents the smallest improvement in score considered clinically significant for the patient.
For this study, the investigators looked solely at the FIM motor scores and the number of days in which patients received physical and/or occupational therapy. Speech therapy was excluded, as the investigators are only looking at motor functional outcomes. The patients were provided with a FIM score rating on admission and on discharge from inpatient rehabilitation. This study examines the change in these scores.
Intervention
The patients were admitted at an inpatient rehabilitation center, accredited by the Commission on The Accreditation of Rehabilitation Facilities, where they received occupational, physical and speech therapy (as needed). The current standard of care in acute inpatient rehabilitation facilities is 3 hours of combined therapy (physical, occupational and speech) per day for 5 days a week. The facility in this study is attempting to increase their standard to 7 days a week for stroke survivors, 2 days greater than the current standard of care. The number of days in which patients received therapy were tracked by a supervisor. Reasons for not receiving therapy 7 days a week were not specifically listed in the data collection, however, include but are not limited to patient refusal, medically unstable, undergoing testing or medical procedure, etc. Because this study is looking at motor outcome, the investigators only tracked the frequency of physical and occupational therapy sessions. Interventions included skilled physical and occupational therapy sessions performed by an occupational therapist, a certified occupational therapy assistant, a physical therapist or a physical therapy assistant. Interventions consisted of personalized treatment sessions including, but not limited to therapeutic exercises, therapeutic activities, neuromuscular re-education, gait training, and activities of daily living training. Advanced technology was utilized for appropriate patients including body weight supported treadmill training, robotic assisted arm training and functional neuromuscular electrical stimulation.
Statistical Analysis
The charts of the patients admitted with a stroke/CVA diagnosis on admission between May 2017- April 2018 in the data system were reviewed. There was a total of 205 admissions during the time period. The charts of the patients (n=19) in the data system with a different diagnosis from the therapy supervisor’s patient records were removed. Four additional medical records were excluded secondary to extenuating social barriers to discharge. The number of charts were then narrowed down further to exclude those coded as a bilateral hemisphere stroke, other, or no paresis, in order to specifically look at the effects of right versus left hemisphere lesions on functional outcomes. They were then further separated into those receiving therapy 7 days a week and those not able to receive therapy 7 days a week. Patients with a stroke diagnosis were scheduled for additional mobility-focused therapy intervention(s) 7 days a week as able.
Data was input into SPSS Statistical Software for analysis. Preparatory analysis was conducted through data cleaning and reviewed for outliers. Baseline statistics between groups (Right stroke vs. Left stroke; 7 days of therapy vs. <7 days of therapy) were compared for demographic information using mean difference tests to ensure that groups are similar, and no baseline differences exist. Linear regression analyses were used to test the efficacy of the protocol for each question. This approach was selected, as it is a more robust analysis due to the relatively small sample size and unequal group numbers in each of the conditions. Separate analyses were conducted for each dependent measure, with the key independent variable being either the side of the brain lesion or the frequency of therapy. The FIM motor score change was the dependent variable for all. To control for baseline performance and to examine change across time, the baseline value for each dependent variable was included in the regression equation. Each regression equation contained 2 independent variables (group assignment and baseline performance). To examine the magnitude of change from baseline to completion in the intervention group, the unstandardized regression coefficient was interpreted with a significance level set at 0.05. Using the unstandardized regression coefficient to examine the incremental change in each outcome measure based on group assignment to the intervention protocol allows interpretation of the amount of improvement noted.
Results
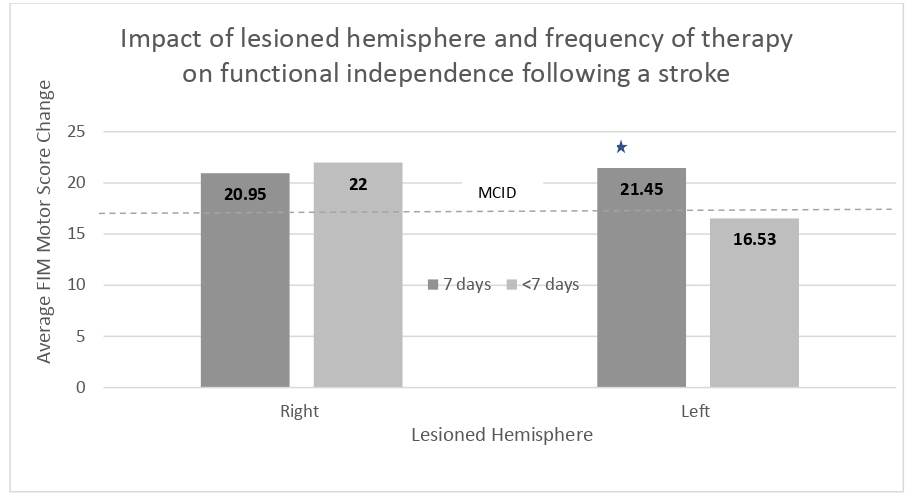
A significant difference was found in FIM motor score change when comparing the frequency of therapy for left hemisphere strokes (left stroke 7 days a week versus left stroke less than 7 days a week) (p=0.021). No significant difference in FIM motor score change was found when comparing the following groups; side of lesioned hemispheres (right vs. left) (p=0.706), frequency of therapy for right hemisphere strokes (right stroke 7 days a week vs. right stroke less than 7 days a week) (p=0.765), or frequency of therapy and side of lesioned hemisphere (right stroke 7 days a week vs. left stroke 7 days a week and right stroke less than 7 days a week vs. left stroke less than 7 days a week) (p=0.138) (Figure 2).
Figure 2: The chart depicts the average Functional Independent Measurement motor score change, comparing the frequency of therapy by hemisphere. The dotted line represents the Minimum Clinically Important Difference for the FIM in the stroke patient population (17 points). The star represents a significance of p>0.05. FIM= Functional Independence Measurement; 7 days=7 days frequency of physical therapy and occupational therapy; <7 days=less than 7 days frequency of physical therapy and occupational therapy; Right=right lesioned hemisphere; Left= left lesioned hemisphere. MCID= Minimally Clinical Important Difference.
The FIM has an established MCID of 17 points for motor score, representing the smallest change that would be considered important by the patient or clinician [19]. The average FIM change was greater than 17 points for almost all groups; total left sided strokes, total right sided strokes, total patients receiving therapy 7 days a week, total patients receiving less than 7 days of therapy a week, left sided strokes receiving therapy 7 days a week, right sided strokes receiving therapy 7 days a week, and right sided strokes receiving therapy less than 7 days a week. The only group in which the average FIM motor score change did not meet the MCID of 17 points were left sided strokes who were provided with less than 7 days of therapy.
Discussion
Similar to Lopes et al., this study found no significant difference in functional independence change between right and left hemisphere stroke survivors [8]. Our research also found similar results to Peiris et al. and Kwakkel et al. demonstrating improved functional independence with increased frequency of therapy sessions [14,15]. However, in this study an increase in the number of therapy sessions was only significantly beneficial for left sided strokes. For right sided strokes, there was no significant improvement in functional independence motor scores with an increase in the number of therapy sessions.
In a study by Denes et al. comparing right and left sided brain lesions, the authors found that those with right sided lesions showed significantly less improvement in ADL performance compared to those with left sided lesions [10]. The authors concluded that the decreased level of independence may be due to unilateral spatial neglect often associated with right sided lesions. This study, however, found no significant difference in functional motor score change between right and left hemisphere, and in fact, showed that the greatest average change in FIM motor score was in right hemisphere lesions when compared to left hemisphere lesions. Although we did not find a similar trend, the common occurrence of unilateral spatial neglect in right strokes may play a role in explaining the lack of significant improvement in FIM scores for right hemisphere stroke patients who received an increased number of physical and occupational therapy sessions.
The findings that there was a significant difference in the FIM motor score of patients with left hemisphere stroke who received 7 days of therapy a week compared to those who received less than 7 days of therapy a week, and the fact that left sided stroke patients who received less than 7 days of therapy a week was the only group that did not show a change that met the minimal clinically important difference threshold from admission to discharge, may suggest that patients who have suffered a left hemisphere stroke require increased frequency of physical and/or occupational therapy sessions to demonstrate functional outcomes similar to those of right sided stroke patients. As discussed previously, common deficits following a left sided stroke include aphasia, difficulty planning and sequencing movements, and trouble processing verbal cues [2,3]. The significant FIM motor score difference noted in those who suffered left hemisphere strokes receiving less than 7 days a week of therapy sessions, compared to those receiving 7 days a week of therapy sessions, may be related to these deficits. The authors also found that all groups met the MCID in the FIM Cognition change scores. As expected, both Left CVA groups showed lower change scores when compared to the Right CVA groups.
With further research we may be able to establish an ideal frequency of combined physical and occupational therapy sessions for stroke survivors based on location of the lesioned hemisphere. The idea that increasing therapy to 7 days a week could produce improved functional independence, comes with further challenges. It may be unrealistic for acute inpatient rehabilitation facilities to provide adequate staffing to treat stroke patients 7 days a week, and the patients, as well, may not be able to tolerate this increased frequency. If increased days of therapy is not possible, increased therapy durations, increased sessions and even group therapy during the current 5 days a week may be a practical alternation. A systematic review by Peiris et al. found that an increase of a minimum of 19 extra minutes of physical therapy a day can led to improved mobility and activity, quality of life and decreased length of stay [14].
Limitations
Limitations of this study include those rating the FIM motor scores. FIM scores were provided by different individuals including physical therapists, physical therapy assistants, occupational therapists, certified occupational therapy assistants and rehabilitation nurses. Scores were not provided by a consistent person from each discipline. Patients were assigned to different teams of therapists and presented with differing levels of impairments. Due to the need for individualized treatments based on the patient’s deficits, it was impossible to provide each person with the same interventions.
The duration of time in total minutes that each patient participated in therapy was not differentiated in this study, only the frequency of therapy in days. This study has a limited sample size, and due to the lack of control and the facility’s’ movement towards increased frequency of therapy for stroke survivors, there was an unequal number of subjects in each group. This study only looked at the lesioned hemisphere of the brain and did not consider the type of stroke, the specific region of the brain impacted, or the severity of the stroke, all of which can play a large role in the patients’ prognosis and recovery.
Conclusion
This study’s findings suggest that acute left stroke survivors may benefit from an intensive frequency of therapy sessions, 7 days a week in an inpatient rehabilitation facility, to improve functional independence. Further research and larger sample sizes are needed to determine any confounding variables which may explain why no significant improvement was noted with increased frequency for right hemisphere stroke patients and to help establish an ideal frequency of therapy based on the lesioned hemisphere, to achieve the greatest functional independence following a stroke.
Acknowledgement
The authors would like to thank Dr. Nicole Dawson of the UCF School of Kinesiology and Physical Therapy for her assistance with this research project.
References
2. O'Sullivan SB, Schmitz TJ, Fulk G. Physical rehabilitation. FA Davis; 2019 Jan 25.
3. Schaefer SY, Mutha PK, Haaland KY, Sainburg RL. Hemispheric specialization for movement control produces dissociable differences in online corrections after stroke. Cerebral Cortex. 2012 Jun 1;22(6):1407-19.
4. Kaplan J, Hier DB. Visuospatial deficits after right hemisphere stroke. American Journal of Occupational Therapy. 1982 May 1;36(5):314-21.
5. Goto A, Okuda S, Ito S, Matsuoka Y, Ito E, Takahashi A, Sobue G. Locomotion outcome in hemiplegic patients with middle cerebral artery infarction: the difference between right-and left-sided lesions. Journal of Stroke and Cerebrovascular Diseases. 2009 Jan 1;18(1):60-7.
6. Stone SP, Halligan PW, Greenwood RJ. The incidence of neglect phenomena and related disorders in patients with an acute right or left hemisphere stroke. Age and Ageing. 1993 Jan 1;22(1):46-52.
7. Kottorp A, Ekstam L, Petersson Lie I. Differences in awareness between persons with left and right hemispheric stroke. Scandinavian journal of occupational therapy. 2013 Jan 1;20(1):37-44.
8. Lopes PG, Lopes JA, Brito CM, Alfieri FM, Rizzo Battistella L. Relationships of balance, gait performance, and functional outcome in chronic stroke patients: a comparison of left and right lesions. BioMed research international. 2015 Jan 1;2015.
9. Bindawas SM, Mawajdeh HM, Vennu VS, Alhaidary HM. Functional recovery differences after stroke rehabilitation in patients with uni-or bilateral hemiparesis. Neurosciences. 2017 Jul;22(3):186.
10. Denes G, Semenza C, Stoppa E, Lis A. Unilateral spatial neglect and recovery from hemiplegia: a follow-up study. Brain. 1982 Sep 1;105(3):543-52.
11. Alemdaroğlu E, Uçan H, Topçuoğlu AM, Sivas F. In-hospital predictors of falls in community-dwelling individuals after stroke in the first 6 months after a baseline evaluation: a prospective cohort study. Archives of Physical Medicine and Rehabilitation. 2012 Dec 1;93(12):2244-50.
12. Beatriz PE, Nascimento C, Marinho C, Oliveira I, Monteiro M, Castro M, et al. Risk factors associated with falls in adult patients after stroke living in the community: baseline data from a stroke cohort in Brazil. Topics in Stroke Rehabilitation. 2014 May 1;21(3):220-7.
13. Ugur C, Gücüyener D, Uzuner N, Özkan S, Özdemir G. Characteristics of falling in patients with stroke. Journal of Neurology, Neurosurgery & Psychiatry. 2000 Nov 1;69(5):649-51.
14. Peiris CL, Taylor NF, Shields N. Extra physical therapy reduces patient length of stay and improves functional outcomes and quality of life in people with acute or subacute conditions: a systematic review. Archives of Physical Medicine and Rehabilitation. 2011 Sep 1;92(9):1490-500.
15. Kwakkel G, Wagenaar RC, Koelman TW, Lankhorst GJ, Koetsier JC. Effects of intensity of rehabilitation after stroke: a research synthesis. Stroke. 1997 Aug;28(8):1550-6.
16. Glasgow Augmented Physiotherapy Study (GAPS) Group. Can augmented physiotherapy input enhance recovery of mobility after stroke? A randomized controlled trial. Clinical Rehabilitation. 2004 Aug;18(5):529-37.
17. Blennerhassett J, Dite W. Additional task-related practice improves mobility and upper limb function early after stroke: a randomised controlled trial. Aust J Physiother. 2004 Jan 1;50(4):219-4.
18. Hsueh IP, Lin JH, Jeng JS, Hsieh CL. Comparison of the psychometric characteristics of the functional independence measure, 5 item Barthel index, and 10 item Barthel index in patients with stroke. Journal of Neurology, Neurosurgery & Psychiatry. 2002 Aug 1;73(2):188-90.
19. Beninato M, Gill-Body KM, Salles S, Stark PC, Black-Schaffer RM, Stein J. Determination of the minimal clinically important difference in the FIM instrument in patients with stroke. Archives of physical medicine and rehabilitation. 2006 Jan 1;87(1):32-9.