Abstract
Granular cell tumor, also known as Abrikossoff’s tumor, is a benign tumor that is relatively rare and is slightly more common in female patients, with a higher prevalence between the fourth and sixth decades of life although it is possible to appear at any age. It can appear in any part of the body but about 45-65% of all the lesions appear in the head or neck areas. Intraoral lesions represent about 70% of these cases. Most of these intraoral lesions appear in the tongue, followed by buccal mucosa and hard palate. Despite the fact that most granular cell tumors are benign, aggressive clinical forms may occur, and there are descriptions of malignant cases, although very few, in medical literature.
We present a case of a granular cell tumor in the medium area of the tongue dorsum in a 43-year-old female patient. It is an example of an oral pathology that is rarely described, and it should have an appropriate medical and surgical approach.
Keywords
Granular cell tumor, Abrikossoff, Medium one-third of dorsum of the tongue
Introduction
Granular cell tumor (GCT) is a rare benign tissue neoplasm of unknown etiology It was first described by Abrikossoff in 1926 [1]. Despite being called granular cell myoblastoma because of its association between granular cells and skeletal muscle, a designation of “granular cell tumor” is now most commonly used [2].
According to immunohistochemistry studies, this lesion originates from neural cells, particularly Schwann cells. Clinically, it is a solitary, painless, slow-growing, well-delimited lesion. In more than 50% of cases, this tumor appears in the head and neck region. The most common location in the oral cavity is the tongue [3]. There is a 2% GCT population reported as malignant. This type of tumor can develop at any age [4]. However, it most often appears between the 4th and 6th decades of life [5]. Although studies suggest a female preference, this prevalence is not unanimously accepted [6].
The ideal treatment for GCTs may be controversial. However, current treatment options are as follows: conservative approach with regular follow-up of tumors less than 10 mm in diameter without evidence of malignancy and surgical excision for tumors more than 20 mm in diameter or benign tumors that cause symptoms or suspected cases of malignancy [6].
Clinical Case
We report a case of a 43-year-old female patient, referred to the stomatology consultation of the Coimbra Hospital and University Centre by her general and family medicine doctor, for the observation of a two-year-old lesion on the tongue. The patient reported that the lesion was painless and slow growing. She had no relevant personal history or relevant usual medication. There were no smoking and/or alcohol habits.
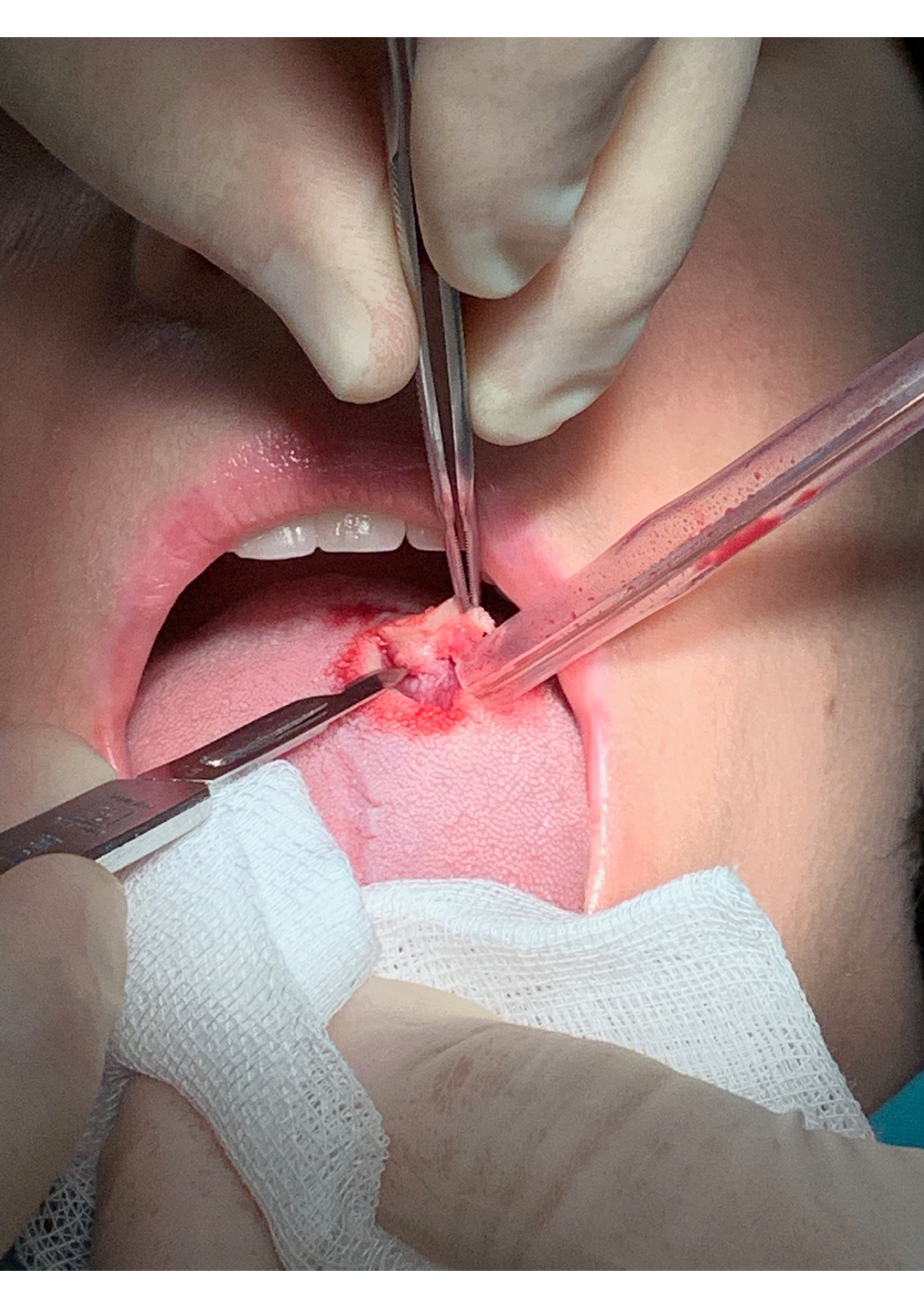
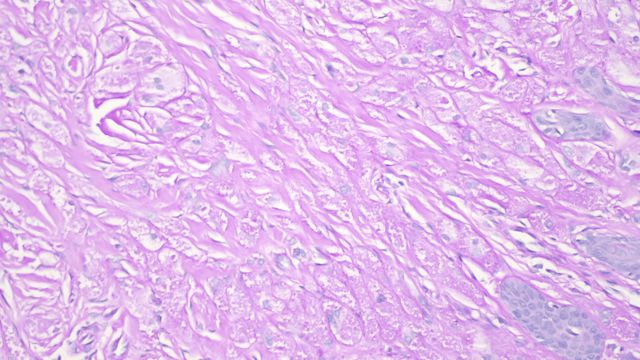
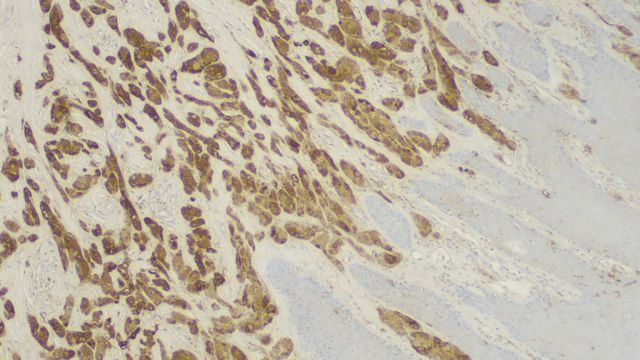
Physical examination revealed a firm, well-circumscribed whitish lesion of about 1.5 cm in diameter, located at the posterior limit of the middle third of the dorsum of the tongue (Figure 1). Thus, an incisional biopsy was performed, whose histological study revealed the diagnosis of granular cell tumor in the dorsal region of the tongue. Given the result, we opted to perform an excisional biopsy under local anesthesia (Figure 2). The macroscopic sample had the dimensions of 1.5 × 0.9 × 0.4 cm, with whitish surface (Figure 3). Its anatomopathological study confirmed the diagnosis of granular cell tumor in the dorsal region of the tongue, and it also reported a submucosal lesion, consisting of proliferation of polygonal cells with large clarified granular cytoplasm PAS+, and with central, oval and monotonous nucleus (Figure 4). Regarding immunohistochemical analysis, the cells had marked and diffuse immunostaining for S100 protein (Figure 5).
Figure 1: Physical examination of the tongue.
Figure 2: Excisional biopsy of the tongue under local anesthesia.
Figure 3: Dimensions of the granular cell tumor, with whitish surface.
Figure 4: Anatomopathological study of granular cell tumor consisting of proliferation of polygonal cells with large clarified granular cytoplasm PAS+, and with central, oval and monotonous nucleus.
Figure 5: immunohistochemical analysis, the cells had marked and diffuse immunostaining for S100 protein.
In the postoperative period the patient evolved without intercurrences and the suture was removed two weeks after surgery. The patient was treated with analgesic therapy, namely ibuprofen 600 mg 12/12 hours and acetaminophen 1000 mg 8/8 hours for five days. There are no signs of recurrence of the lesion 6 months after the surgery, and the patient is regularly checked by her assistant physician at follow-up appointments.
Discussion
Granular cell tumor, also known as Abrikossoff’s tumor, is characteristically asymptomatic, with slow growth and is often accidentally detected. It is characterized by the presence of a small, well-defined, submucosal nodular mass, about 1 to 3 cm in size, of firm consistency and usually covered by intact mucosa [7].
GCTs can develop in almost any part of the body, including skin, subcutaneous tissue, larynx, trachea, bladder, uterus, vulva, and central nervous system, and are most commonly found on the tongue, accounting for almost 30% to 60% of all the GCTs [3].
A wide range of cells has been proposed as the source for granular cells, including histiocytes, myofibroblasts, neural cells, neuroendocrine cells, and undifferentiated mesenchymal cells [1]. Abrikossoff described the lesion composed of lenticular and myoblast tissues, sometimes presenting longitudinal and transverse striations, or containing dark granules.
The most plausible hypothesis for the appearance of this lesion is related to altered Schwann nerve cell metabolism. The persistence of the presence of S-100 protein (pathognomonic marker for peripheral nerve sheath tumors) associated with anatomical similarities with peripheral nerve fibers supports this theory. In this case, the immunohistochemical analysis showed a positive chain for protein S-100, which is considered sufficient for the proposed diagnosis [5]. (Figure 5) Pseudoepitheliomatous hyperplasia (PH) (of the covering epithelium) is present in about 50% of GCT cases [7]. It has been suggested that stimulation of basal cell proliferation occurs through interaction between granular cells and neighboring epithelial cells [8](8). In this case, the presence of labelled HP could initially mimic a squamous cell tumor (SQT). However, SQT is not compatible with the diagnosis due to the absence of several malignant features such as nuclear pleomorphism, mitotic figures or hyperchromatism, for example. The anatomopathological study should be carefully carried out to avoid an incorrect diagnosis of this type of tumor. Up until now, no oral cavity granular cell tumor has been associated with a squamous cell tumor and the dorsum of the tongue is one of the least likely sites for the development this type of cancer [7]. There is a single case of squamous cell tumors involving a granular cell tumor reported by Hee Young Son et al. [9], which leads us to believe that it would be interesting to have more studies on the relationship between granular cell tumors and other tumors.
Clinically, the granular cell tumor can be confused with other connective tissue lesions. Neurofibroma, schwannoma and palisade encapsulated neuroma should be the main considerations for tongue injuries. Tumors of salivary glands, lipoma and other benign mesenchymal neoplasms may present intraorally as asymptomatic nodules similar to the granular cell tumor. Traumatic fibroma is a common reactive lesion that should be included in the differential diagnosis.
Recurrence of GCT, when diagnosed as benign, is uncommon, and is often the result of incomplete excision of the original lesion [10], with 15% of recurrent cases due to incomplete excision being reported [11]. Complete excision of the lesion may not be always possible due to absence of capsule [12]. Therefore, it is advisable to perform an excision with sufficient safety margin (>10 mm) to reduce the probability of recurrence. There are other surgical methods involving the use of laser or electric scalpel that effectively remove the lesion and, if available, could be used. However, they should be preceded by incisional biopsy because the use of these surgical means may increase the risk of compromising the microscopic diagnosis [13].
Conclusion
This case demonstrates the importance of the relationship between clinical and histological and immunohistochemical aspects, all of which are essential to establish the correct diagnosis of GCT [14,15]. In addition, immunohistochemical analysis makes it possible to deepen the knowledge of the etiopathogenesis of GCT, as well as the possible association with other tumors, such as squamous cell tumor. Thus, all available diagnostic tools should be orchestrated to improve the robustness of clinical decision to perform a correct medical-surgical approach to this type of injury.
References
2. Daniels JS. Granular cell tumour of tongue: A case report. The Saudi Dental Journal. 2009 Jul 1;21(2):75-8.
3. Ordonez NG, Mackay B. Granular cell tumor: a review of the pathology and histogenesis. Ultrastructural pathology. 1999 Jan 1;23(4):207-22.
4. Boncoeur-Martel MP, Loevner LA, Yousem DM, Elder DE, Weinstein GS. Granular cell myoblastoma of the cervical esophagus: MR findings. American journal of neuroradiology. 1996 Oct 1;17(9):1794-7.
5. Nishida M, Inoue M, Yanai A, Matsumoto T. Malignant granular cell tumor of the masseter muscle: Case report. Journal of oral and maxillofacial surgery. 2000 Mar 1;58(3):345-8.
6. Miller AS, Leifer C, Chen SY, Harwick RD. Oral granular-cell tumors: report of twenty-five cases with electron microscopy. Oral Surgery, Oral Medicine, Oral Pathology. 1977 Aug 1;44(2):227-37.
7. Dive A, Dhobley A, Fande PZ, Dixit S. Granular cell tumor of the tongue: Report of a case. Journal of oral and maxillofacial pathology: JOMFP. 2013 Jan;17(1):148.
8. Eguia A, Uribarri A, Gay-Escoda C, Crovetto MA, Martínez-Conde R, Aguirre JM. Granular cell tumor: report of 8 intraoral cases. Med Oral Patol Oral Cir Bucal. 2006 Aug 1;11(5):E425-8.
9. Son HY, Kim JP, Ko GH, Lee EJ, Woo SH. Lingual squamous cell carcinoma surrounded by granular cell tumor. Chonnam medical journal. 2012 Apr 1;48(1):65-8.
10. Giuliani M, Lajolo C, Pagnoni M, Boari A, Zannoni GF. Granular cell tumor of the tongue (Abrikossoff's tumor). A case report and review of the literature. Minerva Stomatol. 2004 Jul;53:465-9.
11. Becelli R, Perugini M, Gasparini G, Cassoni A, Fabiani F. Abrikossoff's tumor. Journal of craniofacial surgery. 2001 Jan 1;12(1):78-81.
12. Costa NC, Bertini F, Carvalho YR, Almeida JD, Cavalcante AS. Granular cell tumor presenting as a tongue nodule: two case reports. Journal of medical case reports. 2012 Dec 1;6(1):56.
13. Vinco A, Vettoretto N, Cervi E, Villanacci V, Baronchelli C, Giulini SM, et al. Association of multiple granular cell tumors and squamous carcinoma of the esophagus: case report and review of the literature. Diseases of the Esophagus. 2001 Oct 1;14(3-4):262-4.
14. Poveda R. Granular cell tumour. Medicina oral: organo oficial de la Sociedad Espanola de Medicina Oral y de la Academia Iberoamericana de Patologia y Medicina Bucal. 2004;9(4):362.
15. Sposto MR, Navarro CM, de Andrade CR. Granular cell tumour (Abrikossoff’s tumour): Case series. Oral Oncology Extra. 2006 May 1;42(5):194-7.