Keywords
COVID-19, NLRP3, CD56dim CD16- NK
Introduction
The COVID-19 pandemic caused by the SARS-CoV-2 virus continues to impact populations worldwide, emphasizing the need for improved diagnostic and treatment strategies. Understanding the immune response and identifying early diagnostic markers are crucial in this endeavor. In this comprehensive commentary, we delve into a recent study that investigated the immune cell profiles and NLRP3 gene expression as potential diagnostic markers in COVID-19 patients. By examining the study's objectives, methodology, and findings, we aim to provide a comprehensive analysis of the research and its implications.
Summary of the Study
The study, conducted by researchers in Isfahan, Iran, sought to evaluate the immune cell populations and NLRP3 gene expression in COVID-19 patients compared to healthy individuals. The researchers included 44 hospitalized patients and 20 healthy controls in their study. The findings revealed significant alterations in the immune cell subsets and increased NLRP3 gene expression in COVID-19 patients, suggesting dysregulation of the innate immune response and an activated inflammatory state.
Findings and Significance
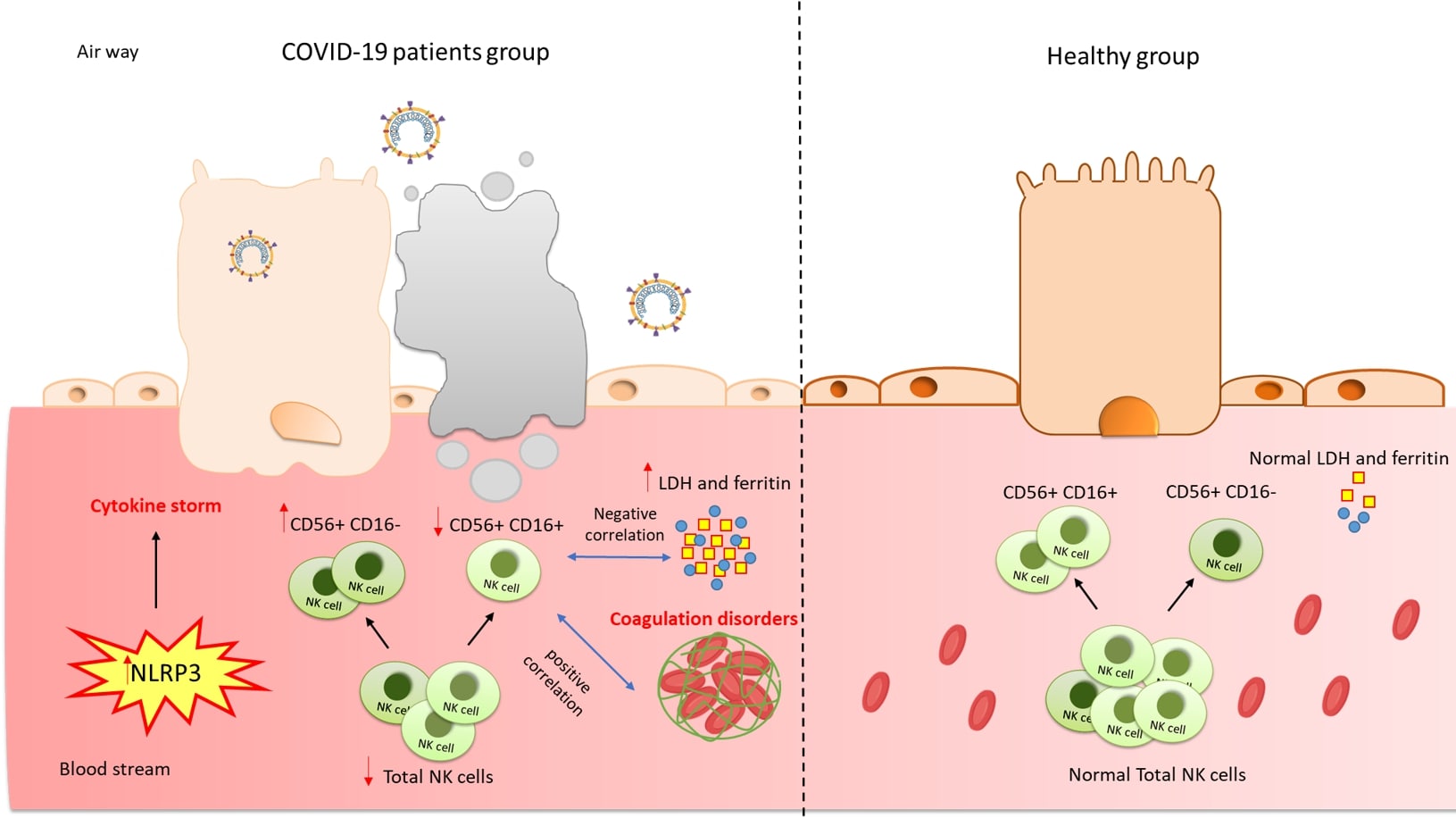
The study demonstrated a significant reduction in natural killer (NK) cell population, particularly in specific NK cell subsets, in COVID-19 patients compared to healthy controls. These findings are consistent with previous studies that have reported impaired NK cell function in severe COVID-19 cases. Interestingly, an unconventional subset of NK cells, CD56dim CD16-, was found to be increased in COVID-19 patients. The increase in CD56dim CD16- NK cells suggest a potential compensatory mechanism or altered NK cell maturation in response to SARS-CoV-2 infection [1].
Additionally, the study reported a significant decrease in natural killer T (NKT) cell population in COVID-19 patients. NKT cells play a crucial role in antiviral immune responses and cytokine production. The observed reduction in NKT cells may contribute to impaired antiviral defense mechanisms and skewed immune responses in COVID-19 patients [2].
Furthermore, the study highlighted a significant increase in NLRP3 gene expression in COVID-19 patients compared to healthy controls. NLRP3 is a key component of the NLRP3 inflammasome, which plays a critical role in the inflammatory response [3]. The upregulation of NLRP3 gene expression suggests an activated inflammatory state in COVID-19 patients, potentially contributing to the cytokine storm observed in severe cases [4,5].
Correlation analysis revealed associations between immune cell percentages and markers of disease severity. NK cell percentages showed a negative correlation with lactate dehydrogenase (LDH) levels, an indicator of tissue damage [6]. CD56+ CD16+ NK cell and NKT cell percentages correlated with ferritin levels, reflecting the involvement of these cells in the hyperinflammatory state observed in severe COVID-19 [7]. CD56brightNK cell percentage and NLRP3 gene expression correlated with international normalized ratio (INR) levels, reflecting coagulation abnormalities commonly seen in severe COVID-19 cases [8]. Notably, NLRP3 gene expression also showed potential as a predictor of hospitalization duration, suggesting its potential utility as a prognostic marker.
Implications and Future Directions
The study's findings have significant implications for the diagnosis, treatment, and understanding of COVID-19. The alterations in NK cell subsets, NKT cells, and NLRP3 gene expression shed light on the immunopathology of the disease and provide potential avenues for therapeutic interventions.
The reduction in NK cell population, especially the decrease in specific subsets, highlights the potential of NK cell-based therapies in COVID-19. Restoring NK cell function or targeting specific NK cell subsets may enhance antiviral immune responses and mitigate disease severity [9]. Furthermore, understanding the factors driving the increase in CD56dimCD16- NK cells could provide insights into NK cell differentiation and their role in viral infections [10].
The decrease in NKT cell population emphasizes the need to explore their functional role in COVID-19. NKT cells are known to regulate immune responses and cytokine production, and their reduction may contribute to dysregulated inflammatory responses in severe cases. Investigating NKT cell-targeted therapies or identifying strategies to modulate NKT cell function could potentially help rebalance immune responses and reduce disease severity [11].
The upregulation of NLRP3 gene expression highlights the involvement of the NLRP3 inflammasome in COVID-19 pathology. Targeting the NLRP3 inflammasome or downstream inflammatory signaling pathways could be a promising therapeutic strategy to dampen the exaggerated immune response observed in severe cases [12]. However, the safety and efficacy of such interventions need to be carefully evaluated.
While this study provides valuable insights, further research with larger cohorts and diverse populations is needed to validate the findings. Collaborative efforts and multi-center studies should be conducted to ensure the generalizability of the results. Additionally, investigating the longitudinal dynamics of immune cell profiles and NLRP3 gene expression during the course of infection and recovery could provide a more comprehensive understanding of COVID-19 immunopathogenesis.
In conclusion, the investigation of immune cell profiles and NLRP3 gene expression in COVID-19 patients contributes to our understanding of the disease's immunopathology. These findings have the potential to improve diagnosis and treatment strategies, ultimately leading to better patient outcomes in the fight against COVID-19. Continued research should focus on validating these markers in larger cohorts, assessing their utility in different clinical settings, and exploring targeted therapies to modulate immune responses and mitigate disease severity.
References
2. De Santo C, Salio M, Masri SH, Lee LY, Dong T, Speak AO,et al. Invariant NKT cells reduce the immunosuppressive activity of influenza A virus–induced myeloid-derived suppressor cells in mice and humans. The Journal of Clinical Investigation. 2008 Dec 1;118(12):4036-48.
3. Allen IC, Scull MA, Moore CB, Holl EK, McElvania-TeKippe E, Taxman DJ, et al. The NLRP3 inflammasome mediates in vivo innate immunity to influenza A virus through recognition of viral RNA. Immunity. 2009 Apr 17;30(4):556-65.
4. Pan P, Shen M, Yu Z, Ge W, Chen K, Tian M, et al. SARS-CoV-2 N protein promotes NLRP3 inflammasome activation to induce hyperinflammation. Nature Communications. 2021 Aug 2;12(1):4664.
5. Rodrigues TS, de Sá KS, Ishimoto AY, Becerra A, Oliveira S, Almeida L,et al. Inflammasomes are activated in response to SARS-CoV-2 infection and are associated with COVID-19 severity in patients. Journal of Experimental Medicine. 2021 Mar 1;218(3).
6. Li C, Ye J, Chen Q, Hu W, Wang L, Fan Y, et al. Elevated lactate dehydrogenase (LDH) level as an independent risk factor for the severity and mortality of COVID-19. Aging (Albany NY). 2020 Aug 8;12(15):15670.
7. Carubbi F, Salvati L, Alunno A, Maggi F, Borghi E, Mariani R, et al. Ferritin is associated with the severity of lung involvement but not with worse prognosis in patients with COVID-19: data from two Italian COVID-19 units. Scientific Reports. 2021 Mar 1;11(1):4863.
8. Rosell A, Havervall S, Von Meijenfeldt F, Hisada Y, Aguilera K, Grover SP, et al. Patients with COVID-19 have elevated levels of circulating extracellular vesicle tissue factor activity that is associated with severity and mortality—brief report. Arteriosclerosis, Thrombosis, and Vascular Biology. 2021 Feb;41(2):878-82.
9. Market M, Angka L, Martel AB, Bastin D, Olanubi O, Tennakoon G, et al. Flattening the COVID-19 curve with natural killer cell based immunotherapies. Frontiers in Immunology. 2020:1512.
10. Hsieh WC, Lai EY, Liu YT, Wang YF, Tzeng YS, Cui L, et al. NK cell receptor and ligand composition influences the clearance of SARS-CoV-2. The Journal of Clinical Investigation. 2021 Nov 1;131(21).
11. Koay HF, Gherardin NA, Nguyen TH, Zhang W, Habel JR, Seneviratna R, et al. Are NKT cells a useful predictor of COVID-19 severity?. Immunity. 2022 Feb 8;55(2):185-7.
12. Shah A. Novel coronavirus-induced NLRP3 inflammasome activation: a potential drug target in the treatment of COVID-19. Frontiers in Immunology. 2020 May 19;11:1021.